
14 Sep Tobias’s Tumor—Successful Treatment of an Acanthomatous Ameloblastoma

Tobias is all smiles after surgery.
Tobias is a happy and energetic 6-year-old Australian Shepherd. Earlier this summer, Tobias’s mom and dad noticed a lump in his mouth. They knew they should not ignore it, so they took action. They took Tobias to our friends at Heritage Animal Hospital in Greenville, WI. Dr. Oberschlake knew this was not normal. He obtained a couple of biopsy samples of the tumor. The diagnosis was an Acanthomatous Ameloblastoma. With this diagnosis, Dr. Oberschlake knew it needed to be completely removed, so Tobias’s parents called Veterinary Dental Specialists of Wisconsin (VDS).
What Is Canine Acanthomatous Ameloblastoma?
Canine Acanthomatous Ameloblastoma (CAA) is a common benign oral tumor in dogs. Benign means it does NOT spread or metastasize to other parts of the body. CAA is classified as a type of odontogenic tumor. Odontogenic tumors are tumors that originate or develop from the same types of cells used in the development and formation of the teeth and periodontal ligament (ligament that holds the tooth in the socket). Some studies have reported CAA being diagnosed in up to 45% of all odontogenic tumors in dogs. Although this is a common oral tumor diagnosis in dogs, it is relatively unique to dogs. It is similar, but slightly different from solid/multicystic ameloblastomas and peripheral ameloblastomas in humans.
CAA is most commonly diagnosed in middle age dogs. Golden Retrievers, Akitas, Cocker Spaniels, and Shelties have an increased prevalence, but any breed can be affected. They can be found on the maxilla or mandible, but there is a preference for the rostral mandible (front of the lower jaw). Although this is a benign tumor, it can be a tough tumor to deal with.
The tumor can develop as a peripheral tumor or arise in the bone. Either form will be located adjacent to or wrapped around a tooth or teeth. The peripheral masses are most common and found in the gingiva (gum tissue). They are usually firm and well adhered to the underlying bone. The tumor will often have an irregular surface, although some may be smooth. When they have bony invasion, they can often grow to hard swellings in the bone and dive deep within the bone. It can invade cortical, medullary, or alveolar bone, leading to lysis or destruction of the bone. In time, teeth may become displaced and appear shifted or loose.
Diagnosing Oral Tumors in Dogs
Diagnosis requires more than visualizing a lump or swelling. Unfortunately, many other tumors can appear similar. Other types of odontogenic tumors can look like this, but so can some malignant (cancerous) tumors, such as Squamous Cell Carcinoma. The best way to obtain a diagnosis is via biopsy. Since these tumors can sometimes look like other tumors, it is very important to have a large, representative sample. The sample should be reviewed by a pathologist familiar with oral pathology. Imaging such as intra-oral dental radiographs and/or CT imaging can be useful in determining location and potential bony involvement.
Oral Tumor Treatment Options for Dogs
Once the diagnosis is made, treatment decisions need to be considered. There are many treatment options available. En bloc surgical excision (removal) is considered the “Gold Standard” for CAA. Typically, one-centimeter margins are recommended. This means the removal of one-centimeter of normal tissue all around the tumor. With complete removal, the odds of recurrence or regrowth are extremely low. Recent reports have shown that smaller surgical margins may still be successful and have a low risk of recurrence. In situations where the tumor cannot be removed, radiation therapy can be another option to explore, although there are potential long-term side effects with this approach. Intralesional injections of Bleomycin are still discussed in the literature, but localized side effects are not uncommon, thus it has fallen out of favor.
Treating Tobias’s Oral Tumor

Well-defined tumor at the left mandibular first molar.
When Tobias visited us on the day of surgery, it was agreed that he would be anesthetized and the entire mouth would be evaluated. A Complete Oral Health Assessment and Treatment (COHAT) plan was developed. The plan was to completely excise (remove) the tumor with appropriate surgical margins.
When Tobias was anesthetized, the teeth were cleaned, and the entire mouth was evaluated. The tumor was at the gum tissue of the left mandibular first molar and measured 16mm by 18mm by 9mm in size. Intraoral dental radiographs of the tumor were taken and the rest of the mouth. Cone Beam CT imaging was also performed to allow three-dimensional views of the tumor. Imaging showed focal bone loss centered around the base of the tumor.

CT image showing the extent of the marginal rim excision performed on Tobias.
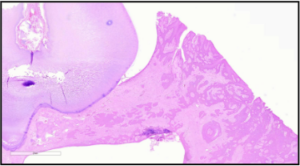
Microscopic view of the tumor. Image courtesy of SOPA and Dr. CIndy Bell, DVM, DipACVP.
Removal of the tumor involved what is called a “marginal rim excision”. Based on the size and location of the tumor on the lower jaw, one-centimeter margins could be obtained and still leave enough jaw bone to allow for function and alignment. The mandible has a large canal near the bottom of the jaw that contains a major artery, vein, and nerves. Cutting into this can cause major bleeding or nerve damage. A piezotome with a bone cutting tip was used to score and cut the bone, staying well clear of the tumor. A big advantage of this device is that it is minimally damaging to vessels and nerves.
After surgery, Tobias had a lot of stitches, but they would dissolve in a few weeks. Due to the amount of jaw bone removed, he was given strict instructions to avoid hard chewing and tug-of-war. He was sent home the same day with pain relievers and instructed to be on soft food for a couple of weeks. The tumor was submitted to an oral pathologist, Dr. Cindy Bell of Specialty Oral Pathology for Animals, who confirmed the diagnosis and reported good surgical margins and complete removal.
At a recheck two weeks later, Tobias was healing well and back to a nice smile. The risk of recurrence is extremely low and he has an excellent prognosis.
References:
Goldschmidt SL, Bell CM, Hetzel S, Soukup J. Clinical Characterization of Canine Acanthomatous Ameloblastoma (CAA) in 263 dogs and the Influence of Post-surgical Histopathological Margin on Local Recurrence. J Vet Dent. 2017 Dec;34(4):241-247. doi: 10.1177/0898756417734312. Epub 2017 Oct 4. PMID: 28978273.
Liptak, J.M. Cancer of the Gastrointestinal tract. In: Withrow and MacEwen’s Small Animal Clinical Oncology, 6th Edition; 2019
4. Fiani N, Verstraete FJ, Kass PH, Cox DP. Clinicopathologic characterization of odontogenic tumors and focal fibrous hyperplasia in dogs: 152 cases (1995-2005). J Am Vet Med Assoc. (2011) 238:495–500. 10.2460/javma.238.4.495
Goldschmidt SL, Bell CM, Hetzel S, Soukup J. Clinical Characterization of Canine Acanthomatous Ameloblastoma (CAA) in 263 dogs and the influence of post-surgical histopathological margin on local recurrence. J Vet Dent. (2017) 34:241–7.
Arzi B, Verstraete FJ. Mandibular rim excision in seven dogs. Vet Surg. 2010 Feb;39(2):226-31. doi: 10.1111/j.1532-950X.2009.00630.x. PMID: 20210971.
Murphy BG, Bell CM, et al. Odontogenic Tumors. In: Veterinary Oral and Maxillofacial Pathology, 1st Ed. 2019.


